New research published today suggests that high levels of lipoprotein(a) may be linked to an 18-20% increased risk of cardiovascular disease in people with hypertension, but not in those without high blood pressure.
High blood pressure is a well-known risk factor for cardiovascular disease, and lipoprotein(a) is a type of inherited “bad” cholesterol that can also increase the risk of cardiovascular disease, according to lead author Rishi Rikhi.
In this new study they “found that among people with hypertension who have never experienced a stroke or heart attack before, lipoprotein(a) seems to increase the risk of cardiovascular disease and risk of a major cardiovascular event like heart attack or stroke.”
Hypertension is a major cardiovascular disease risk factor. Hypertension was defined in this research as systolic blood pressure (SBP) of 140 mmHg or higher, diastolic blood pressure (DBP) of 90 mmHg or the use of blood pressure medication. The American Heart Association revised its definition of hypertension in 2017 to include readings of 80 mmHg or higher on the bottom or a top reading of 130 mmHg or higher. According to earlier research, having both hypertension and a lipid imbalance, or dyslipidemia, significantly raises a person’s chance of developing cardiovascular disease. Less is known about the potential impact of lipoprotein(a) on cardiovascular disease risk in individuals with hypertension, according to the study’s authors.
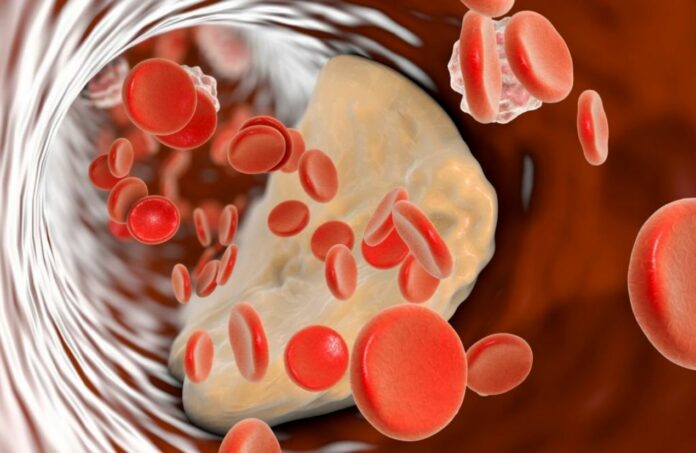
Lipoproteins, which are composite molecules consisting of protein and fat, are what transport cholesterol through the bloodstream. Low-density lipoprotein, also known as LDL, high-density lipoprotein, also known as HDL, and lipoprotein(a), also known as Lp(a), are the subtypes of lipoproteins. Similar to LDL cholesterol, lipoprotein(a) cholesterol may accumulate and lodge in the blood vessel walls, raising one’s chance of having a heart attack or stroke.
The study utilized health data from the Multi-Ethnic Project of Atherosclerosis (MESA) investigation, an ongoing community-based study of subclinical cardiovascular disease in the United States, which means the illness is detected before clinical signs and symptoms appear. MESA is a research project that started in 2000 and is continuing monitoring participants in six different U.S. locations: Baltimore, Chicago, New York, Los Angeles County, California, Forsyth County, North Carolina, and St. Paul, Minnesota. Nearly 7,000 individuals are a part of it. All trial participants were free of cardiovascular disease at the time of enrolment.
The 6,674 MESA participants who had their blood pressure and lipoprotein(a) levels measured as well as those for whom there was recorded cardiovascular disease event data during MESA’s follow-up exams in approximately 2001, 2003, 2004, 2006, 2010, and 2017 as well as during telephone interviews every 9 to 12 months to gather interim data on new diagnoses, procedures, hospitalizations, and deaths were included in the current study. Individuals in the research came from a variety of racial and ethnic backgrounds. Of the n=791 participants, 38.6% self-identified as white, 27.5% as African American, 22.1% as Hispanic, and 11.9% as Chinese American. Also, more than half of the group (52.8%) were women.
The participants were then divided into groups according to their blood pressure readings and lipoprotein(a) levels in order to assess the possible relationship between hypertension and cardiovascular disease development:
- Group 1: lipoprotein(a) levels less than 50 mg/dL and no high blood pressure (2,837 people).
- Group 2 (615 people): lipoprotein(a) levels of 50 mg/dL or higher and no high blood pressure
- Group 3 (2,502): lipoprotein(a) levels below 50 mg/dL and high blood pressure
- Group 4: lipoprotein(a) levels of less than 50 mg/dL and high blood pressure (720 people).
Heart events like heart attacks, cardiac arrest, strokes, and deaths due to coronary artery disease were recorded throughout the course of a mean follow-up of around 14 years.
The results of the study are:
- Overall, 809 people had a cardiovascular disease-related incident.
- Hypertension status was significantly affected by lipoprotein(a) levels (meaning it was not due to chance).
- Compared to Group 1, which had low lipoprotein(a) levels and no high blood pressure, Group 2, which had higher lipoprotein(a) levels and no high blood pressure, did not have a higher risk for cardiovascular disease events.
- Heart problems struck less than 10% of those in either Group 1 (7.7%) or Group 2 (8%).
- All of the people in Groups 3 and 4 had high blood pressure, and compared to Group 1, they had a statistically significant higher chance of having a heart attack or stroke.
- Cardiovascular disease events occurred in about 16.2% of those in Group 3 (lower lipoprotein(a) levels and hypertension) and in approximately 18.8% of those in Group 4 (higher lipoprotein(a) levels and hypertension).
“We found that the overwhelming amount of cardiovascular risk in this diverse population appears to be due to hypertension,” says Rikhi, adding, “additionally, individuals with hypertension had even higher cardiovascular risk when lipoprotein(a) was elevated. The fact that lipoprotein(a) appears to modify the relationship between hypertension and cardiovascular disease is interesting, and suggests important interactions or relationships for hypertension, lipoprotein(a) and cardiovascular disease, and more research is needed.”
Everyone can improve their cardiovascular health by adhering to Life’s Essential 8 as outlined by the American Heart Association: eating healthy food, being physically active, not smoking, getting enough sleep, maintaining a healthy weight, and controlling cholesterol, blood sugar, and blood pressure levels. The American Heart Association says that cardiovascular disease kills more people each year in the U.S. than all types of cancer and chronic lower respiratory disease put together.
The study had some limitations, such as potential selection bias from participants dropping out due to its long-term duration, which could disproportionately affect one of the four subgroups.
Furthermore, participants may have been misclassified if they acquired hypertension during the study’s follow-up period.
The findings were published today in the journal Hypertension
Source: 10.1161/HYPERTENSIONAHA.122.20189
Image Credit: Getty