This novel barrier may also help to partially explain why so-called breakthrough infections are so common and why smell loss is far more frequently linked to these infections than pulmonary symptoms.
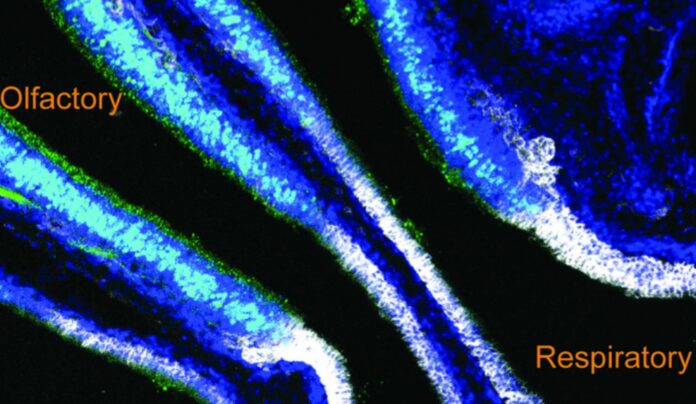
Duke researchers discovered a previously unknown barrier that separates the bloodstream from smelling cells in the upper airway of mice, most likely to protect the brain.
However, this barrier also serves to block some of the body’s bigger immune system components, which may reduce the efficiency of vaccines.
According to lead author Ashley Moseman, an assistant professor of immunology at Duke School of Medicine, the olfactory cells that line the nose make sense to have a protective barrier since they provide a direct route to the brain’s olfactory bulb, thereby making them extensions of the brain.
However, the new barrier, named the BOB (blood-olfactory barrier) by his team, maybe blocking antibodies from reaching the mucous on the nose’s surface, the first barrier a virus meets.
The team wanted to learn more about how the immune system protects the upper respiratory tract. They did this by giving mice a virus called vesicular stomatitis virus, or VSV, which is known to get into the central nervous system. Once breathed, VSV easily infects olfactory detecting cells and multiplies quickly, making it to the brain’s olfactory bulb in just one day. Although it can cause paralysis and death, a T cell reaction generally eliminates it.
“VSV is excellent at infecting olfactory sensory neurons, and when it can do that, it will get into the brain,” says Moseman. “Even if you have antibodies in circulation, the blood-olfactory barrier prevents these antibodies from reaching the airway surface, and VSV will get into the brain.”
They were interested in learning more about how one illness could guard against another. They discovered that while the BOB blocked the protection provided by circulating antibodies, it did let antibody-secreting plasma cells to enter olfactory tissues and create neutralising antibodies there.
The findings were published in the journal Immunity today.
Although the researchers weren’t specifically interested in this issue because of COVID, it is well-documented that the SARS-CoV-2 virus infects olfactory cells and renders many affected people unable to smell. They now believe that this novel barrier may help to partially explain why so-called breakthrough infections are so common and why smell loss is far more frequently linked to these infections than pulmonary symptoms.
“The reason that COVID infections typically stay in the upper airways and less commonly reach the lungs of vaccinated people may involve this gap in immune protection,” Moseman adds.
“You could have a situation where you have perfectly good (amounts of) antibody in circulation from a COVID vaccination, but these antibodies are prevented from reaching the olfactory cells,” adds Moseman. “You’d be protected against severe pulmonary disease, which is great, but you could still have these replicating events going on in the olfactory epithelium because the systemic antibody doesn’t get there. This is obviously unpleasant for the individual, and may contribute to continued community spread.”
The discovery, according to Moseman, also brings his team closer to explaining why many vaccines fail to induce antibody-secreting B cells into tissues, whereas infections can.
“Vaccines create antibody-secreting cells that make antibody and give you a nice blood antibody titer, but those cells don’t necessarily enter and protect these tissues,” he adds. “Antibodies that are in circulation don’t get to the olfactory surface where they can protect against the viral infection.”
More effective vaccinations might result from knowing how the immune system distinguishes between an infection and a vaccination, according to Moseman.
More effective vaccinations might result from knowing how the immune system distinguishes between an infection and a vaccination, according to Moseman.
To find the BOB in other animals and people, the researchers must first have a deeper understanding of the components that make up the BOB.
It could be very difficult technically to study this little area in humans, according to Moseman.
“If you understood what constitutes it, what factors maintain it and all these kinds of things in the mouse, then it will be a little bit easier to try to transfer that knowledge and look for it in human tissue.”
“We think it’s certainly plausible that this would exist in humans. We just haven’t actually been able to test it directly,” Moseman adds. “There are a lot of questions.”
Source: 10.1016/j.immuni.2022.08.017
Image Credit: Ashley Moseman Lab, Duke University
You were reading: The Reason COVID Prevents Vaccines From Being More Effective – Even If You Have Antibodies