The World Health Organization says that antimicrobial resistance is one of the top 10 threats to global public health, and scientists have been working hard to find new ways to treat the most dangerous drug-resistant infections.
Research conducted by a University of Maryland researcher in partnership with the National Institute of Allergy and Infectious Diseases reveals that treating drug-resistant illnesses by lowering virulence rather than by aiming to completely eradicate the bacteria may be an effective solution.
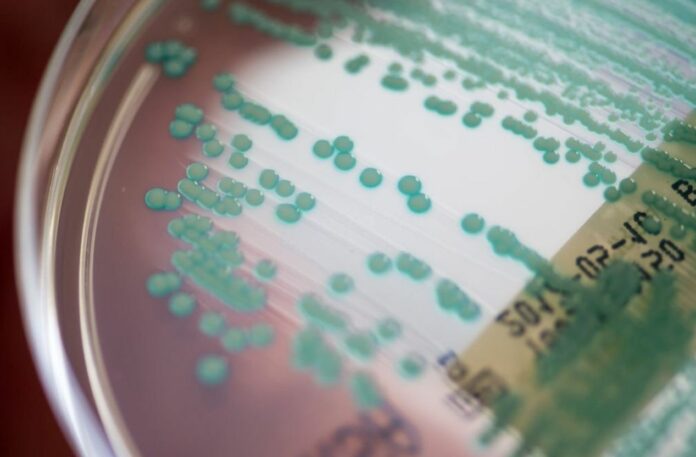
The results of their investigation demonstrated how two proteins help the methicillin-resistant Staphylococcus aureus (MRSA) bacteria release the toxins that cause illness.
According to the findings, treatments that target these two proteins may be able to deactivate MRSA, making it less lethal and maybe even harmless. In addition to lowering the potential for antibiotic resistance, this strategy also has other benefits.
The study, which was released today in the Proceedings of the National Academy of Science, speculates that additional bacteria may have similar capabilities, opening the door to a novel method of treating bacterial infections.
Lead author Seth Dickey says that they were looking for a different method to tackle MRSA. They aimed to comprehend the disease-causing mechanism of the bacterium with the goal of directly interfering with its virulence factors. By disabling it, they hope to eliminate the need to worry about its ability to evade antimicrobial agents.
When a drug treatment kills some but not all of the bacteria cells, this is called antimicrobial resistance. If the bacteria have a time to recolonize, they often have some natural resistance, making the subsequent infection more resistant to antibiotics. Super-bugs like MRSA and multi-drug resistant TB are the result of this unintended selective breeding.
This kind of selective breeding could be stopped if there was a way to treat infections that made them less dangerous without killing them. This has been hard to do with MRSA because the bacteria makes a lot of different kinds of toxins.
Identifying each mechanism and disabling it is quite difficult. Dickey and his colleagues made the decision to focus on how the cells leak the toxins into their host rather than how the cells manufacture the toxins.
According to research conducted by Dickey and colleagues, two proteins operate as ferries, carrying toxin molecules over the bacterial cell membrane.
It was not known, however, why there were two transporter proteins or how they worked. Without this knowledge, researchers are unable to create treatments that stop the release of toxins.
Dickey and his colleagues genetically altered each kind of transporter and then watched MRSA cells produce toxins to better understand the process at work.
They found that a particular transporter protein binds to hydrophilic, or water-loving, toxins that are floating in the cytoplasm of the cell and transports them across the cell membrane.
When that transporter wasn’t there, hydrophilic toxins kept building up inside MRSA cells, where they are harmless to both MRSA and any possible host.
When the team took out the hydrophobic, or water-repelling, second transporter protein, toxins began to build up in the cell. This is important because these toxins tend to move by themselves from the watery cytoplasm to the oilier cell membrane.
And that’s where both host cells and MRSA cells get hurt by MRSA toxins. As a result, MRSA cells are harmed by their own hydrophobic toxins in the absence of the second transporter protein.
This means that in the future, therapies that target one transporter could diminish virulence, while therapies that target the other transporter might do the same while simultaneously acting as antibiotics.
The study’s results are important for more than just MRSA. The researchers discovered that many other bacteria contain genes for building a dual transport protein system similar to the one they discovered in MRSA when they examined the genomes of several other bacteria.
Source: 10.1073/pnas.2211689120
Image Credit: Getty