Despite the fact that the Omicron variant is spreading over the world, public health experts have highlighted that the number of Covid patients in hospitals is often lower than during past pandemic surges.
That isn’t the situation in the United States, where the number of coronavirus patients in hospitals has surpassed all-time highs.
On January 11, according to numbers from the Department of Health and Human Services, 145,982 Americans were hospitalized with the virus, breaking the previous high recorded in January 2021.
On Thursday, US President Joe Biden was scheduled to announce plans to send military medical staff to six of the states that have been struck the hardest by the surge of patients.
Surges have also been reported in hospitals across most of neighboring Canada, with Quebec reporting a pandemic high last weekend.
What is happening, and why is United States’s experience so far different from that of South Africa and Europe?
What numbers reveal?
Let’s start with this graph, which shows how many people were hospitalized with Covid-19 in various nations throughout the pandemic. It is a ratio of infected hospital patients per million people that has been adjusted to account for population size.
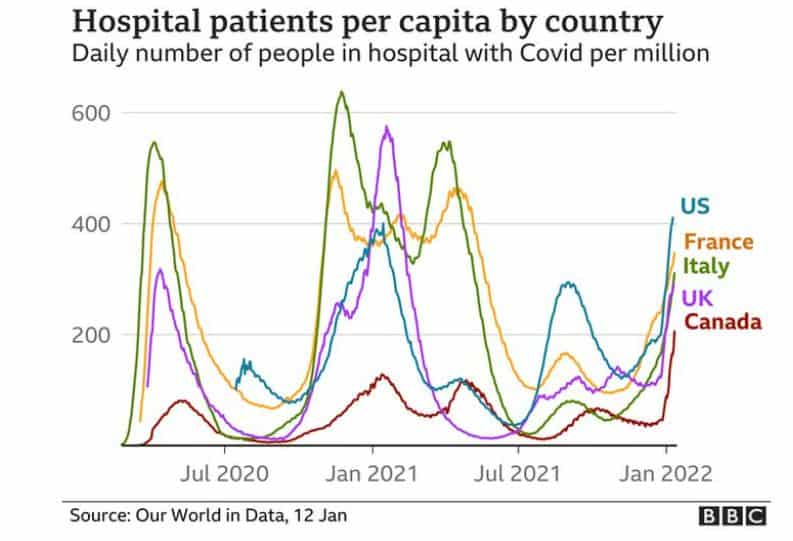
A wave of Covid came to each country at different times. These peaks show when each country was hit by new waves, like the first outbreak and influx of patients to hospitals, last winter’s surge or the summer spike caused by the Delta variant.
For example, the green line depicts how hard Italy was affected during the start of the pandemic and again last year, peaking at 638 infected people per million inhabitants on November 23, 2020.
Due to Omicron, every country on the right side of the figure has seen a significant increase in Covid-infected hospital patients. What’s more fascinating is comparing the current rates in each country to the prior peaks.
The number of patients in hospital with Covid in Italy, France, and the United Kingdom is substantially lower than in prior rounds. On January 10, 291 people with coronavirus per million were admitted to hospitals in the United Kingdom. The ratio was 576 per million just over a year ago. On the same day in France, the ratio was 347 per million, down from a peak of 490 in November.
In the United States, on the other hand, as of January 9, there were 411 US Covid-19 patients per million people in hospitals, beating the previous high of 400 per million recorded on January 14, 2020.
Similarly, as of January 11, 206 individuals per million were in hospital in Canada, compared to previous highs of 118 in April and 128 in January 2021.
As a result of mandatory testing in hospitals, some patients with Covid-19 in the US and Canada may have been found only as “incidental” cases. Doctors say that the overwhelming number of patients needing care has put a strain on the health care system.
Situation of hospitals in the United States?
According to reports from hospitals across the United States, the influx of infected patients has intensified the strain on facilities already overburdened by the pandemic.
This surge, according to Dr Juan Reyes, the director of hospital medicine at George Washington University in Washington DC – which is one of the cities in the United States with the highest per capita hospital admissions rate – “has been a lot more challenging” than prior ones.
“The challenge that we’re feeling now is that it’s happening at a larger volume and things are a little bit tighter,” he told the BBC. “The difference now is a lot of fatigue, on healthcare workers and the population at large.”
Despite less severe infections among patients, Dr Lewis Rubinson, chief medical officer at Morristown Medical Center in New Jersey, estimated that the current admissions spike is “about twice the size” of the previous high in the spring of 2020.
Part of the rise in numbers, he said, can be due to greater testing of everyone who enters the hospital for any reason. Newly admitted patients in the United States, the United Kingdom, and Canada are all tested for Covid, regardless of what brought them to the hospital.
Still, “the overall impact on hospitals by the sheer numbers is tremendous,” he added. “[If] you take off even a third of those, it’s still an enormous amount of patients that we’re tackling.”
National Health Service officials in the United Kingdom believe that this number of so-called accidental Covid cases is between 20 and 30 percent of all cases.
Compared to South Africa
In South Africa, where the Omicron strain was first discovered in November, researchers discovered that individuals infected with Omicron are less likely to be hospitalized and recover faster.
While there are no current statistics on the number of Covid patients in hospitals per capita, many South African hospitals stated that the number was substantially lower than during past surges.
According to the International Journal of Infectious Diseases, the number of infected patients at the Steve Biko Academic Hospital in Tshwane was around half of what had been reported before mid-November.
Researchers believe that due to earlier Covid-19 waves and low vaccination coverage in South Africa, many inhabitants had already been exposed to the virus and had developed some immunity.
Compared to Canada?
According to Dr. Donald Vinh, an infectious disease specialist at McGill University Health Centre in Montreal, as many as half of all new hospital admissions in Quebec – and other parts of Canada – are among the “inadequately vaccinated.”
“As a percentage of the population, it’s a low number. Maybe 10% of the eligible population are not doubly vaccinated,” he said. “They tend to be clustered in urban dense spots. When you have highly transmissible variants and it can affect an inadequately vaccinated population, this leads to ongoing propagation and the high community transmissions we’re seeing.”
Dr. Vinh argues that, like the United States, Canada has a “incongruent” public health strategy when it comes to Covid-19.
“In other words, there isn’t a single unified method in how we’re going to do things across the board,” he added. “It’s more regional than national, and because of that you have gaps. The consequences of that are people getting hospitalised.”
Why the US is so different?
There are various reasons why the rate of Covid patients in hospitals in North America is higher than in most other parts of the world, according to experts.
According to Professor David Larsen, an epidemiologist and global health expert at Syracuse University in New York, the US population differs significantly from those of Europe and South Africa.
“We have an older population than South Africa. That’s a big one,” the professor said. “[The US] is kind of similar in age structure to Europe. But there’s also a less healthy population than in Europe.”
Dr. Larsen pointed out that the United States has greater rates of hypertension and obesity than most other nations, both of which are comorbidities that raise the risk of Covid.
It is “incredibly frustrating,” Dr. Larsen continued, to hear Americans underestimate the ongoing threat of Omicron and expect that, like South Africa, the United States will soon emerge from the current surge of the virus.
“The seasonality is also different,” he added. “Omicron’s surge through South Africa was during their summer, and it’s hitting us in winter when we know more people gather indoors and there’s more transmission…it’s going to be bad.”
According to Dr Mark Cameron, an associate professor of population and quantitative health sciences at Case Western University in Ohio, “a perfect storm” of Covid-19, comorbidities, unequal access to healthcare, and anti-vaccine sentiment is wreaking havoc on the United States’ health care system.
“When all of that ‘perfect storm’ nature of vulnerabilities that are unique to the US combine, you’ve got an outbreak of the virus that can quickly lead from increased cases to increased hospitalisations, which tax the local hospitals and health community.”
The United States has a vaccination rate of just over 63 percent, which is significantly lower than the United Kingdom (71 percent), Italy, and France (both 75 percent ). Almost 79 percent of the population in Canada is totally protected.
Is Delta variant culprit?
Doctors also warn that the high number of hospital admissions in the United States and Canada could be linked to the Delta variant’s prevalence in many regions.
According to a study published in August in The Lancet Infectious Diseases that looked at 43,000 people in the UK, the Delta variant had a risk of hospitalization that was more than quadruple that of prior strains.
While Dr. Monica Gandhi, an infectious diseases specialist and professor at the University of California, San Francisco, believes Delta patients make up a considerable part of Covid-19 hospital admissions in the United States, she admits that determining the real proportion is difficult.
“We don’t know how much Delta there is,” she said. “What the US has started to do is look at the number of new infections and sequences. Omicron is 95% of new infections, but we don’t know how much Delta we still have around.”
Some patients “are sicker and some are less sick” in Dr. Gandhi’s own hospital, she noted, “and that feels very much like Delta and Omicron are both there.”
What comes next?
Researchers in many nations believe that the Omicron variety has begun to fade, possibly signaling the end of the Covid-related increase in hospital patients.
According to a computer model developed by experts at the University of Washington, the number of daily cases in the United States will peak at 1.2 million on January 19. Some researchers believe that cases will peak sooner rather than later.
In the short term, however, analysts anticipate that hospitals in the United States and Canada will continue to be strained by rising patient numbers, even as they decline in other nations.
“The situation is bad. There’s really no other word to describe it,” Dr. Vinh added. “I would love to start seeing an inflection point that tells us we’re at the plateau, but right now all I’m seeing is a hill. It’s not even a hill anymore. It’s a wall.”
Dr. Larsen, for his part, added he believes that the United States needs “more urgency around systemic change” to move past Covid-19.
Both Dr. Cameron and Dr. Gandhi in the United States think that hospital admissions will peak in February or March.
“It still could make for a miserable winter. I think that for the next month, life is going to be really hard in schools and hospitals,” Dr. Gandhi warned.
Image Credit: Getty
You were reading: Why ‘Covid Hospitalization Rate’ is higher in the United States than in most other parts of the world
